Blocked Milk Duct
What is a Blocked Milk Duct?
The expression blocked milk duct is a non-medical term which covers a range of lactational breast issues. A blocked milk duct is not a defined diagnosis and not an expression used by many experienced health professionals.
Most breast surgical and diagnostic practices only see lactating mothers when a breast abscess is suspected, so may not be a good source of advice for blocked milk ducts. An initial point of contact for advice on who to see next should be your GP or Maternal Health Nurse.
Blocked Milk Duct: Symptoms and Signs
When lactating mothers have a breastfeeding problem they may use the expression blocked milk duct for a range of concerns about feeding which include:
- an area of lumpiness in the breast with or without pain which is persisting after a feed.
- redness and firmness in an area of the breast.
- Mastitis - this is usually accompanied by fever and feeling unwell.
The implications of using the term blocked milk duct is that something mechanical is blocking one or more milk ducts and this can be unblocked in some way.
Failure of one part of the breast to adequately drain milk for a time is not seen as a defined physical blockage in a duct, but rather due to stasis of milk, or swelling in the breast tissue which may cause pressure on part of the duct system.
Blocked Milk Duct Possible Causes
A blocked milk duct may occur if your baby starts to sleep through the night or if you drop a feed. Tops and bras that put pressure on the breast area should be avoided and you should ensure you rest, eat well and stay healthy while breastfeeding. These are important factors which could be potential causes of blocked milk ducts. In most cases, a blocked milk duct will not progress to Mastitis. If it does not resolve promptly it should not be ignored.
Relieving a Blocked Milk Duct:
- Feed on the affected side, altering feeding positions and feeding frequently.
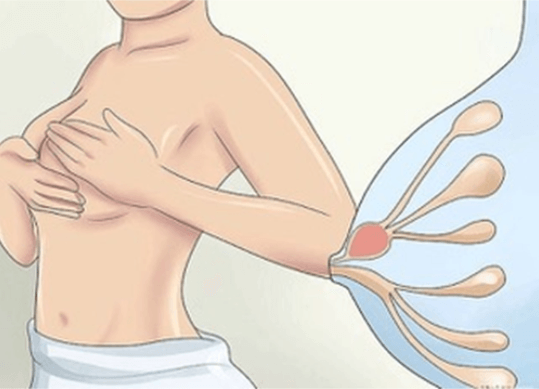
- Very gentle massage lumps towards the nipple during and after feeds.
- Apply warmth to the area before a feed.
- Cool packs may be applied to the area following a feed to relieve pain and inflammation.
- See your medical adviser if you cannot clear the lump/blockage within a few days, or sooner if you begin to feel unwell.
Focal Engorgement
This means one segment of the breast may not empty completely after a feed and feels like an area of thickening with or without pain. This may resolve with the next feed leaving a normal lactating breast.
Mastitis
Mastitis is similar to focal engorgement but with erythema and more pain, may occur over a wider area and often with temperature and flu-like symptoms.
Mastitis Remedies
Mastitis may require antibiotics unless it is mild and settles promptly with the next feed. If you suspect Mastitis you should promptly see your GP for further direction.
Breast Abscess
A breast abscess is where an area of Mastitis does not respond to antibiotics, usually noticed as a painful red breast lump.
Breast Abscess Remedies
If a breast abscess develops a fluid centre with pus, it may require a needle aspiration to remove the pus, so the breast can settle with the antibiotics. It is rare for a breast abscess to require operation under general anaesthetic with a drain tube inserted, as even large abscesses can be managed with repeated aspiration under local anaesthetic.
Does a Blocked Milk Duct Require Medical Treatment?
A blocked milk duct may not require any treatment as most areas of focal engorgement will settle with subsequent feeding or gentle massage. If the same area of the breast is a recurring problem it is wise to check your feeding position and technique with a lactation consultant. Your GP or Maternal Health Nurse will be able to advise if this is required.
A blocked milk duct is no harm to your baby but could potentially affect milk supply, if it is an ongoing issue.
Role of an Ultrasound for Blocked Milk Ducts
Do I need a breast ultrasound if I suspect a Blocked Milk Duct?
This is only indicated if a possible abscess is suspected. A mammogram is not indicated.
It is important to be aware that with breastfeeding, problems usually disappear on weaning and even abscess aspiration will not leave any problem with the breast ducts and glandular tissue, so there will be no scarring. There is no association with breast cancer.
Helpful Resources for Blocked Milk Ducts or Persistent Breast Issues
- Maternal Health Nurse (Maternal and Child Health Line, provide support and advice to Victorian families with children from birth to school age (five years old), 24 hours a day, 7 days a week- 13 22 29)
- General Practitioner
- Lactation Consultants
- Australian Breastfeeding Association (Helpline 1800 686 268)
Who is Affected by Breast Cysts?
Breast Cysts are common in women in the age group of 35-50. They usually cease with menopause, but are common in women taking Hormone Replacement Therapy (HRT).
Approximately 7% of women may have a palpable cyst at some point of their lives.
Diagnosis of Breast Cysts
Breast cysts can be impalpable, asymptomatic and are usually identified by an incidental finding on routine imaging.
On ultrasound, cysts appear as well-defined round or oval anechoic (black) lesions.
Atypical cysts though asymptomatic may require aspiration under the guidance of ultrasound and a sample will be sent for cytological assessment.
Typical breast cysts are not cancerous, and cysts do not increase breast cancer risk. Asymptomatic cysts with typical features of a benign cyst do not require treatment.
Draining Breast Cysts
The cystic fluid can be drained using a fine needle. Cyst fluid can vary in colour and consistency. The fluid can be clear or coloured- yellow, green, orange, or black.
Treatment of Symptomatic Cysts
Women with symptomatic cysts (causing significant discomfort) can be considered for aspiration to provide symptomatic relief, either under clinical or ultrasound guidance.
A palpable lump that has the typical features of a simple cyst on ultrasound does not require aspiration to confirm the diagnosis.
Surgery is rarely recommended for treating cysts.
Fat Necrosis
Fat necrosis occurs due to trauma (sudden injury) or a specific injury to the breast. Breasts are made up of lobules, ducts, glandular, fibrous, and fatty tissue.
The damaged area of breast tissue can lead to a lump formation known as fat necrosis. Necrosis refers to cell death. The damage to the fatty breast tissue commonly occurs following breast surgery, including breast reduction and breast reconstruction, or radiotherapy to the breast.
Most women diagnosed with fat necrosis have no history of any specific injury at all.
Fat necrosis appears like a firm painless lump, but some women may have tenderness or even pain. The skin around the lump may look red, bruised, or occasionally dimpled.
At times fat necrosis, can cause the nipple to retract inwards. Although fat necrosis is benign, it can sometimes look like breast cancer. These lumps of breast tissue may appear as malignant breast tumours on mammograms and other imaging studies.
Therefore, for a proper diagnosis full triple assessment is required.
Fat necrosis often resolves on its own. If the lump does not disappear over time, or increases in size, a small surgery may be recommended to remove the lump. Fat necrosis can be observed in women of any age. It is a benign breast condition and does not increase breast cancer risk.