Breast Imaging Victoria News

At Breast Imaging Victoria, we believe breast health starts with knowledge. That’s why we’re proud to offer patients access to iPrevent - an evidence-based breast cancer risk assessment tool developed by the Peter MacCallum Cancer Centre and endorsed by the The Royal Australian College of General Practitioners (RACGP) . 🔎 What is iPrevent? iPrevent is a free, online tool designed to help women understand their personal breast cancer risk. It combines detailed personal and family history with validated scientific models to estimate an individual’s risk of developing breast cancer over their lifetime. ✨ Why does it matter? Not all women face the same level of risk. Age, breast density, family history, lifestyle factors, and genetic background all influence breast cancer risk. iPrevent makes it easier to translate those risk factors into meaningful, personalised information. 💬 At BIV, how do we use it? Patients have the option of completing the iPrevent risk assessment while waiting for their imaging appointment. This information helps our radiologists and multidisciplinary team personalise future imaging surveillance and make sure you receive the right level of monitoring for your risk profile. 🩺 Benefits of iPrevent at BIV: - Empowers patients with a clearer understanding of their breast cancer risk - Supports conversations with your GP or breast specialist - Guides decisions on screening frequency (annual vs biennial) and imaging type (mammogram, ultrasound, contrast-enhanced mammography) - Provides peace of mind by turning risk factors into a practical plan 📣 Breast Imaging Victoria is committed to being more than just an imaging clinic — we’re a partner in your long-term breast health journey. Tools like iPrevent help us make care more proactive, personalised, and effective . You are welcome to contact us if you have further questions.
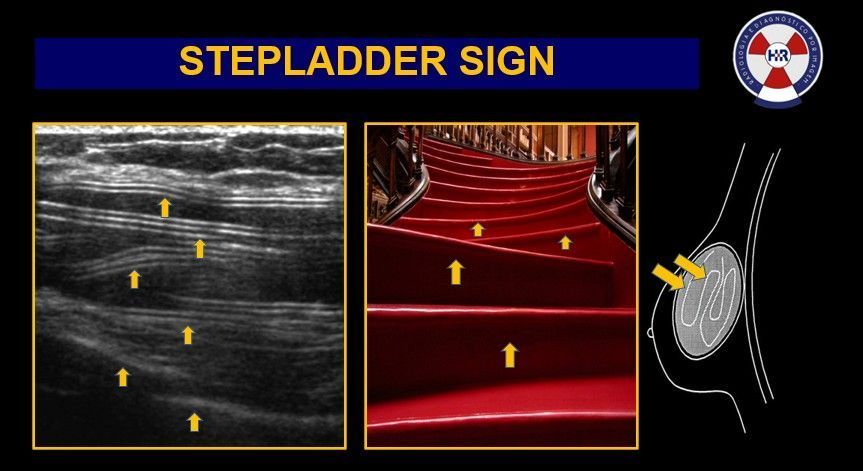
While mammograms remain a crucial part of breast screening, ultrasound is the workhorse when it comes to monitoring implant health and detecting complications. At Breast Imaging Victoria, we routinely use high-resolution ultrasound in combination with mammography to give a clearer, more complete picture. Here’s what ultrasound can help with: ✅ Silent implant ruptures It can detect small tears or leaks -even if you don’t have symptoms. For example you can get ruptures within your implant shell (intracapsular ruptures) which might not be physical noticeable but can be seen under ultrasound. A common sign is the stepladder sign as seen in the image posted. ✅ Capsular contracture Ultrasound helps measure the thickness of scar tissue forming around your implant, indicating how severe the contracture may be. ✅ Implant positioning issues We can identify signs of bottoming out, rotation, displacement or herniation. ✅ Peri-implant complications From fluid (seroma), blood (hematoma), or infection (abscess), ultrasound helps us catch issues early -before symptoms worsen. ✅ Cancer screening In augmented or dense breasts, ultrasound is often more accurate in detecting small breast masses or suspicious lesions. ✅ Avoiding unnecessary MRIs Ultrasound provides a cost-effective, radiation-free alternative for ongoing implant surveillance in many cases. ✅ Procedure guidance Ultrasound also allows precise needle guidance if a biopsy or aspiration is needed near the implant. ✨ At BIV, we tailor imaging to each patient. For women with implants and remaining breast tissue, we usually recommend both mammogram + ultrasound (unless your referral says otherwise). If you’ve had reconstruction post-mastectomy, ultrasound alone is usually appropriate. 📣 Have breast implants? Talk to your GP about getting referred to a specialist breast imaging clinic. Early detection applies to everyone - and we’re here to help you stay one step ahead.
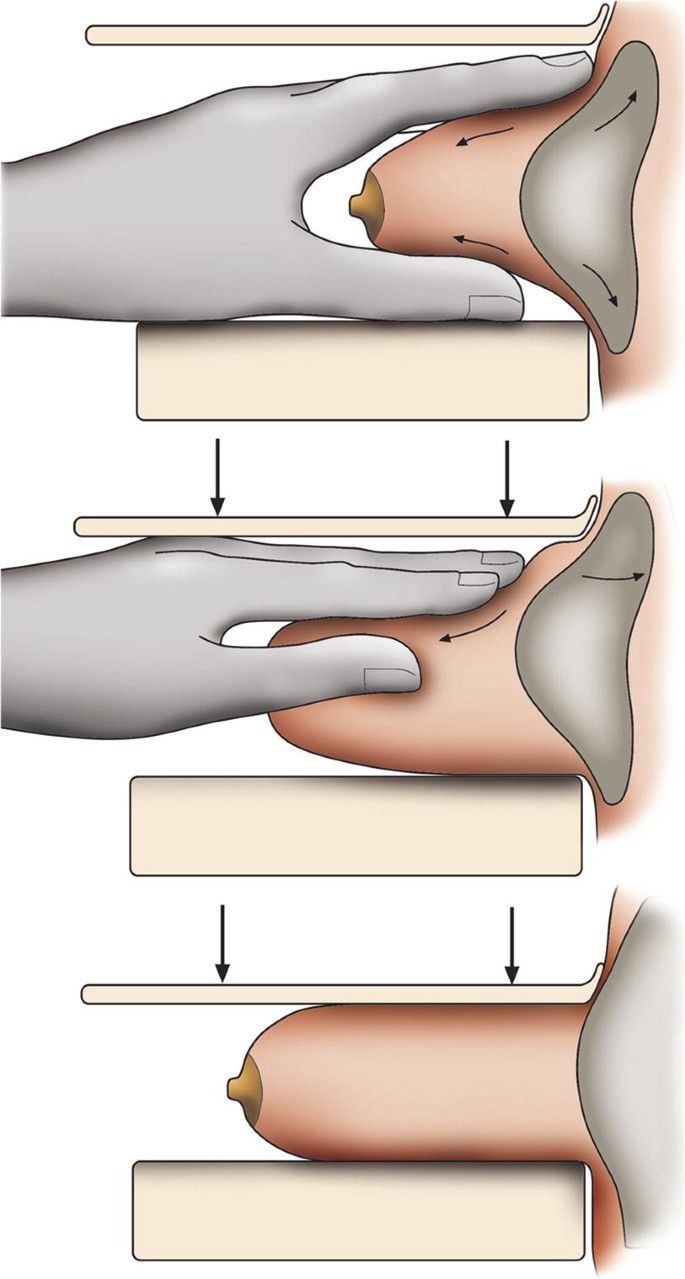
At Breast Imaging Victoria, we regularly perform specialised mammograms for women with breast implants using implant displacement views (the Eklund technique), to ensure we capture as much breast tissue as possible — especially what’s hidden behind the implant. This allows us to see up to 85% of the breast tissue, regardless of implant type or size. 👉This specialised technique gently pushes the implant back towards the chest wall while the breast tissue is pulled forward and imaged separately. This ensures clearer, more accurate results. It may sound uncomfortable, but don’t worry — we apply soft, controlled compression to keep things as comfortable as possible while ensuring diagnostic quality. Many patients tell us they feel very little during the displaced views because the implant buffers the pressure. 🩻 Our radiographers are trained in this technique and perform it daily. These extra views are important because standard mammograms may not always see around or through the implant — especially when looking for subtle changes or early signs of cancer. 👩⚕️ Whether you have saline or silicone implants, both are handled the same during mammography — neither is better or worse in terms of compression or image clarity. ✨At BIV, we tailor every scan to the individual. For those with implants and breast tissue (not post-mastectomy), we usually combine mammogram and ultrasound to give the clearest picture possible. 🗓 The current recommendation is for women aged 45–70 to have a mammogram every 2 years - and that includes women with implants. If you have risk factors, screening may begin earlier or happen more frequently. Talk to your GP. Have questions? We’re here to help you understand your options and feel confident in your care.
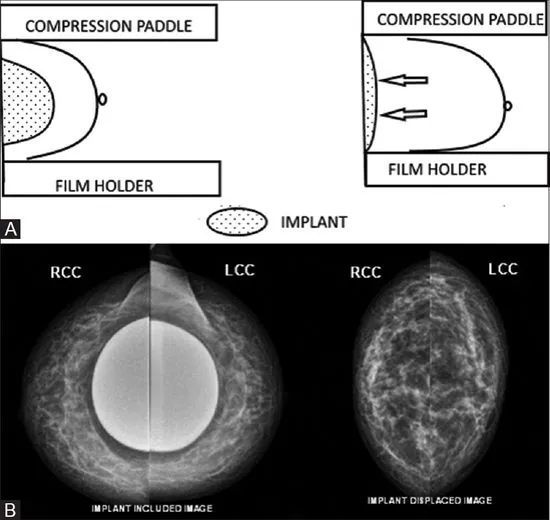
Yes, you can and should have mammograms if you have breast implants. At Breast Imaging Victoria, we routinely image patients with implants and tailor each exam for your safety and comfort. Mammograms are still a great tool to assess breast tissue, even if you have implants. We use minimal compression and implant-displacement views (to focus on breast tissue) to get clear images without compromising the integrity of the implant. In most cases, we also recommend ultrasound alongside your mammogram for the most complete picture. If you’ve had breast reconstruction post-mastectomy, we generally use ultrasound only. Have questions? Just ask. Our team is here to guide you every step of the way.

Ever been told you need a stereotactic biopsy and wondered why it’s different (and sometimes more costly) than an ultrasound biopsy? Stereotactic biopsies are highly specialised procedures used when abnormalities (like microcalcifications) are only visible on a mammogram, not ultrasound. Using 3D mammographic guidance, the radiologist can precisely target and biopsy these tiny areas. But what makes it so specialised? - Advanced equipment and technique: The procedure relies on high-tech machinery, fine targeting, and a trained team. - Time and precision: It often takes longer than an ultrasound biopsy due to positioning, targeting, and post-biopsy imaging. - Sometimes two biopsies are needed: If your doctor identifies two separate areas, each will require its own sterile field, separate equipment, and careful repositioning. This is effectively two procedures in one -which is why the cost doubles. Always ask if you’re unsure. Understanding the "why" behind your imaging journey empowers you to make informed decisions.
Do you know your breast density? You should. At Breast Imaging Victoria, we’ve been routinely reporting breast density for several years—because knowledge is power when it comes to your breast health. Now, BreastScreen Victoria has also begun including breast density information in their reports, and we welcome this important step forward. 🔎 Why does breast density matter? Dense breasts can make it harder to detect cancer on a mammogram and may slightly increase the risk of developing breast cancer. Knowing your density helps guide the right follow-up—whether that’s adding ultrasound or even contrast-enhanced mammography. 📋 At BIV, we tailor your imaging based on your density, personal history, and risk factors. It's not one-size-fits-all—your screening should be as unique as you are.
PSA! GP Guideline Updates! New symptom? Here’s how to investigate it properly. Cancer Australia has released updated guidance on investigating new breast symptoms, and it's an important reminder of how age influences imaging choices. 🔎 Key Takeaways: Women 35 years and over: Begin with a mammogram, followed by an ultrasound if needed. Under 35 years : Ultrasound is the first-line imaging modality. Add a mammogram only if findings are suspicious, indeterminate, or don’t match the clinical picture. Suspicious lumps: GPs should include a detailed history and are encouraged to discuss with the radiologist on the day. This may lead to further targeted imaging such as contrast-enhanced mammography. MRI is not recommended as routine first-line imaging, but may be used later in complex or inconclusive cases in specialist consultation. At Breast Imaging Victoria, we follow these evidence-based protocols closely and welcome GP collaboration to ensure the best outcomes. Please remember to book mammograms first in patients aged 35+, unless clinical judgement suggests otherwise. 📄 View the full guide here: https://lnkd.in/gEMSKieu
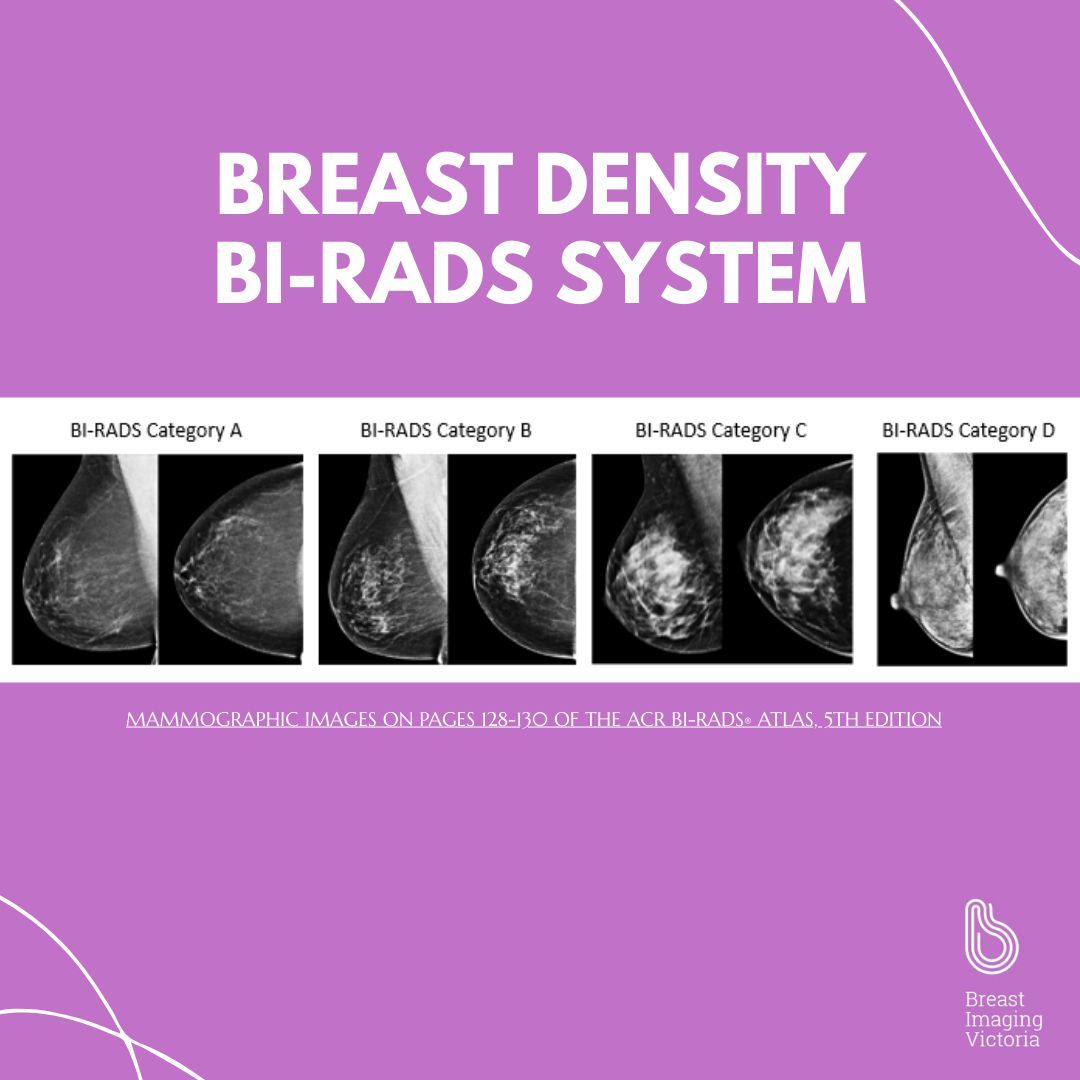
We’re pleased to hear that BreastScreen Victoria is now reporting on breast density - a welcome move toward transparency and personalised care. At Breast Imaging Victoria, we’ve been routinely reporting breast density for several years, because we’ve long believed that breast health starts with knowledge. 🧠 What does it mean to have dense breasts? Breast density refers to the ratio of fibroglandular (dense) tissue to fatty tissue in the breast. It’s reported using the BIRADS classification: - A (fatty) - B (scattered fibroglandular) - C (heterogeneously dense) - D (extremely dense) Around 40–50% of women fall into the C or D categories. Higher density can: - Slightly increase breast cancer risk - Make cancers harder to see on standard mammograms 🩺 What this means for GPS: GPs now play a vital role in guiding patients with dense breasts toward appropriate follow-up, especially if other risk factors are present. - Review patient history, age, and family risk - Consider ultrasound or contrast-enhanced mammography where appropriate - Help patients understand that density is not a diagnosis, but part of informed screening 🔍 What this means women : Knowing your breast density empowers you to make informed choices. If you’ve been told you have dense breasts, speak to your GP about whether additional imaging may benefit you. At Breast Imaging Victoria, we support both patients and GPs with a full suite of tailored breast imaging services—and we’re proud to lead the way in comprehensive breast density reporting. 💬 Knowledge is power. Let’s keep the conversation going.
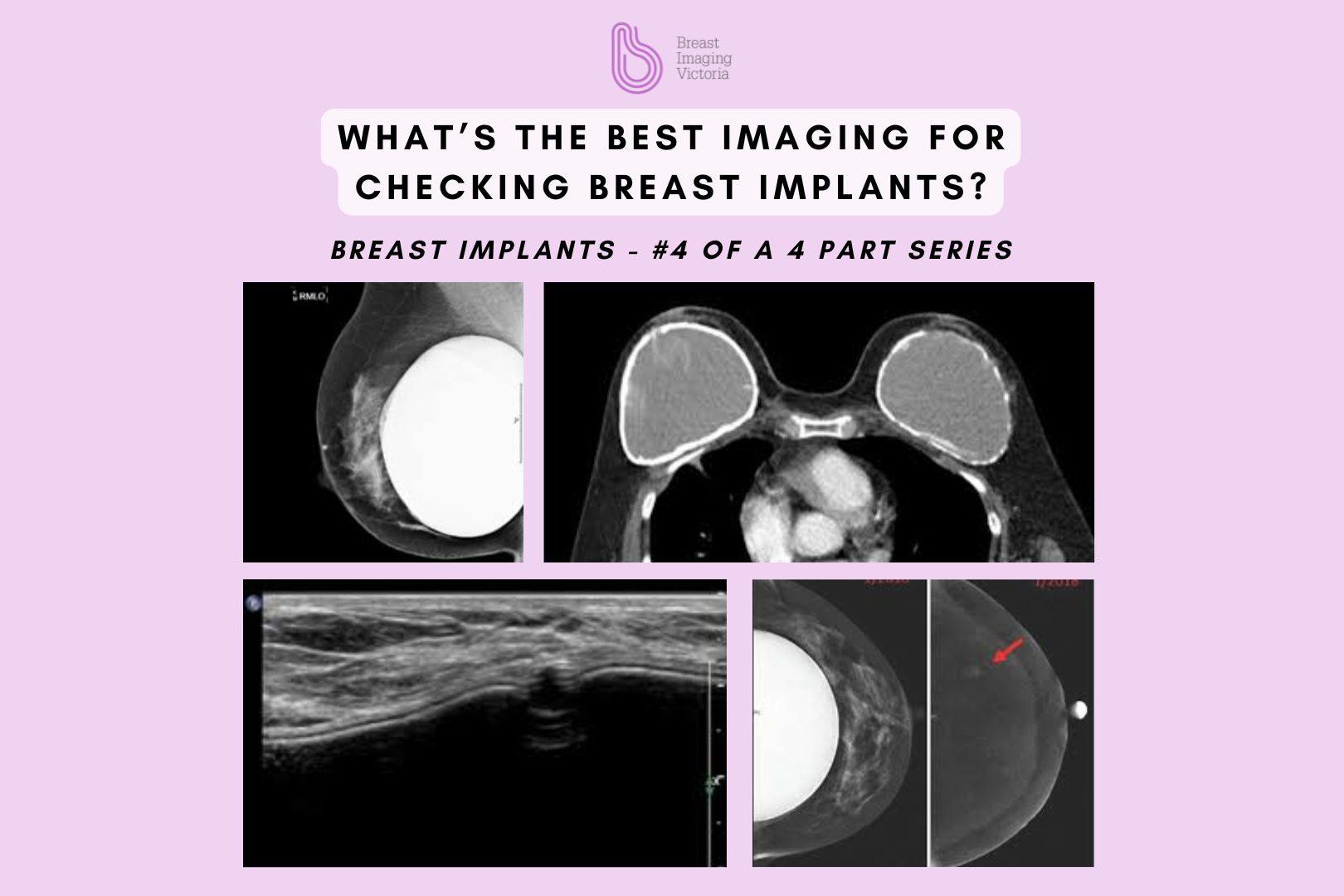
Mammogram, ultrasound, or MRI—which is best for assessing breast implants? At Breast Imaging Victoria, we typically perform both a mammogram and an ultrasound when assessing patients with breast implants—unless the referral specifies otherwise. This dual approach ensures a thorough evaluation of both the breast tissue and implant. 👉 Important note: This applies to patients with cosmetic breast implants and remaining breast tissue. For patients with implants following mastectomy, where there is no remaining breast tissue, ultrasound alone is usually sufficient. What Each Modality Offers: Mammogram : Vital for screening the surrounding breast tissue. We use soft compression to safely stabilise the breast and implant for clear imaging. Ultrasound : The first-line tool for assessing implant integrity and identifying any signs of leakage or rupture. MRI : In certain cases, if there are concerns about implant rupture or complex findings, an MRI may be requested externally for further clarification. Not sure which imaging applies to you or your patient? Contact our team for guidance.
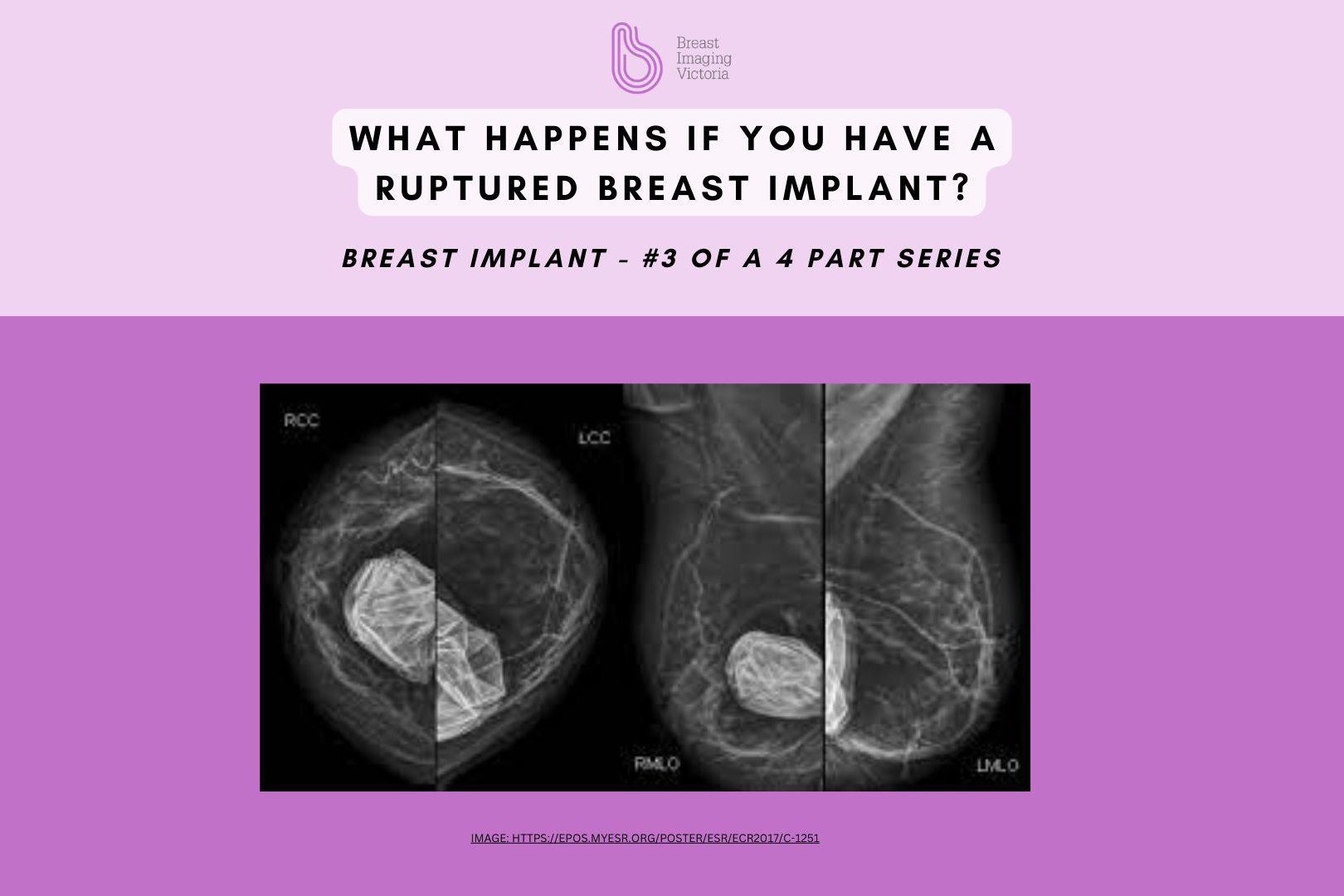
Welcome back to #3 of our 4 part series on breast implants. What happens if a breast implant ruptures? Here’s what you need to know. Saline Implant Rupture: The body absorbs the saline solution, and the breast deflates. Silicone Implant Rupture (Silent Rupture): May not show obvious symptoms, making imaging essential. Symptoms to Watch For: Pain, swelling, changes in shape, or hardening of the breast. How Do We Check for Rupture? Mammogram: Used to assess surrounding breast tissue with soft compression to stabilise the area. Ultrasound: First-line imaging for implant integrity and leaks. MRI: The gold standard for detecting silent ruptures when symptoms are unclear. If rupture is confirmed, your breast surgeon will discuss options, which may include implant removal or replacement. If you have concerns about your implants, book an imaging assessment to get clarity and peace of mind.
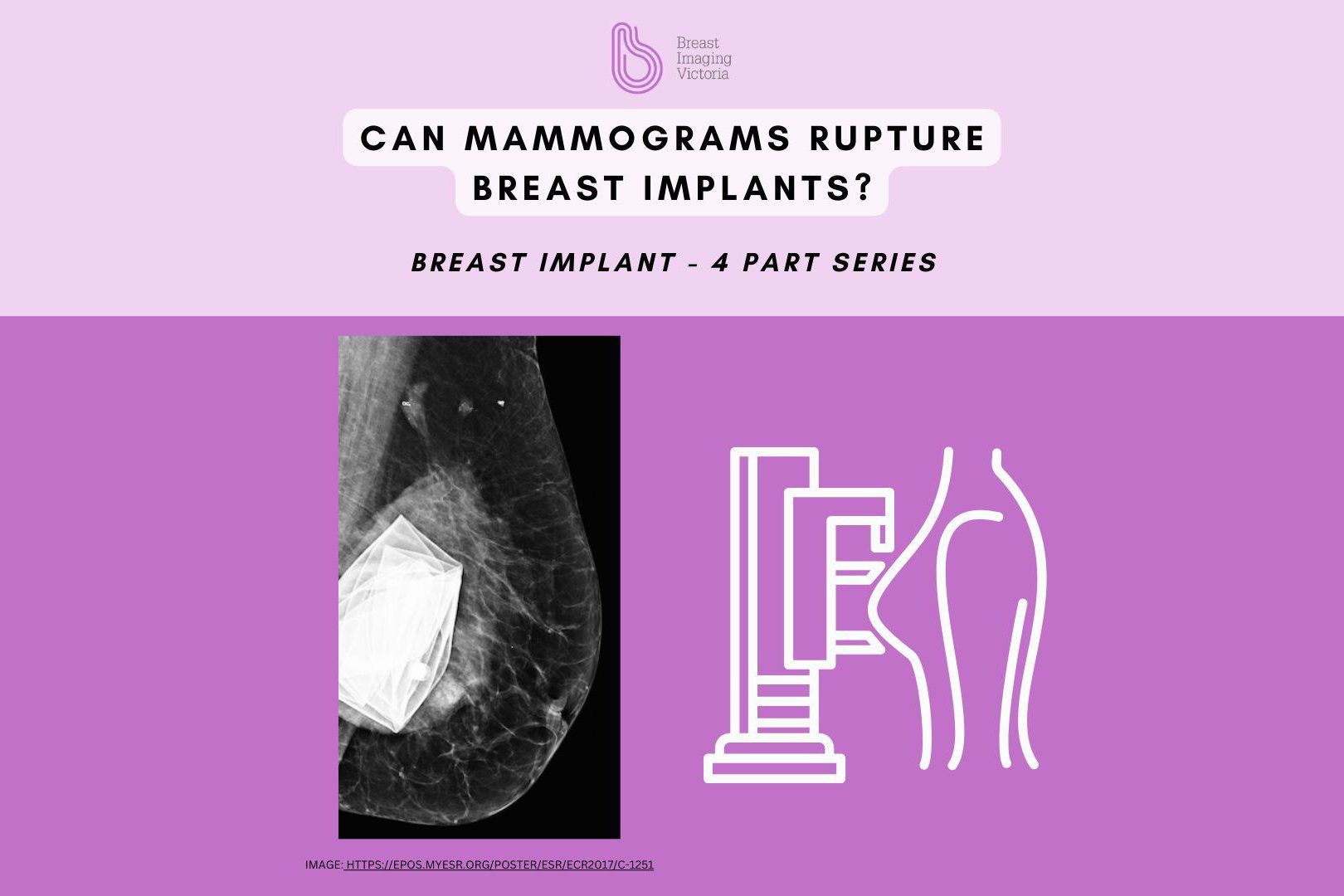
Can Mammograms Rupture Breast Implants? One of the biggest concerns we hear from patients with breast implants: Can a mammogram rupture them? Let’s break it down. - Mammograms do NOT cause implant rupture when performed correctly. - Soft compression is applied, ensuring the implant stays in place while allowing the best possible image of the surrounding breast tissue. - Implant displacement views move the implant out of the way to focus on the breast tissue itself. - If an implant is already weakened, a mammogram may detect the issue, rather than cause it. - If you experience symptoms like hardness, shape changes, or pain, additional imaging (ultrasound or MRI) may be required. Have concerns about imaging with implants? Speak to our team for personalised advice.
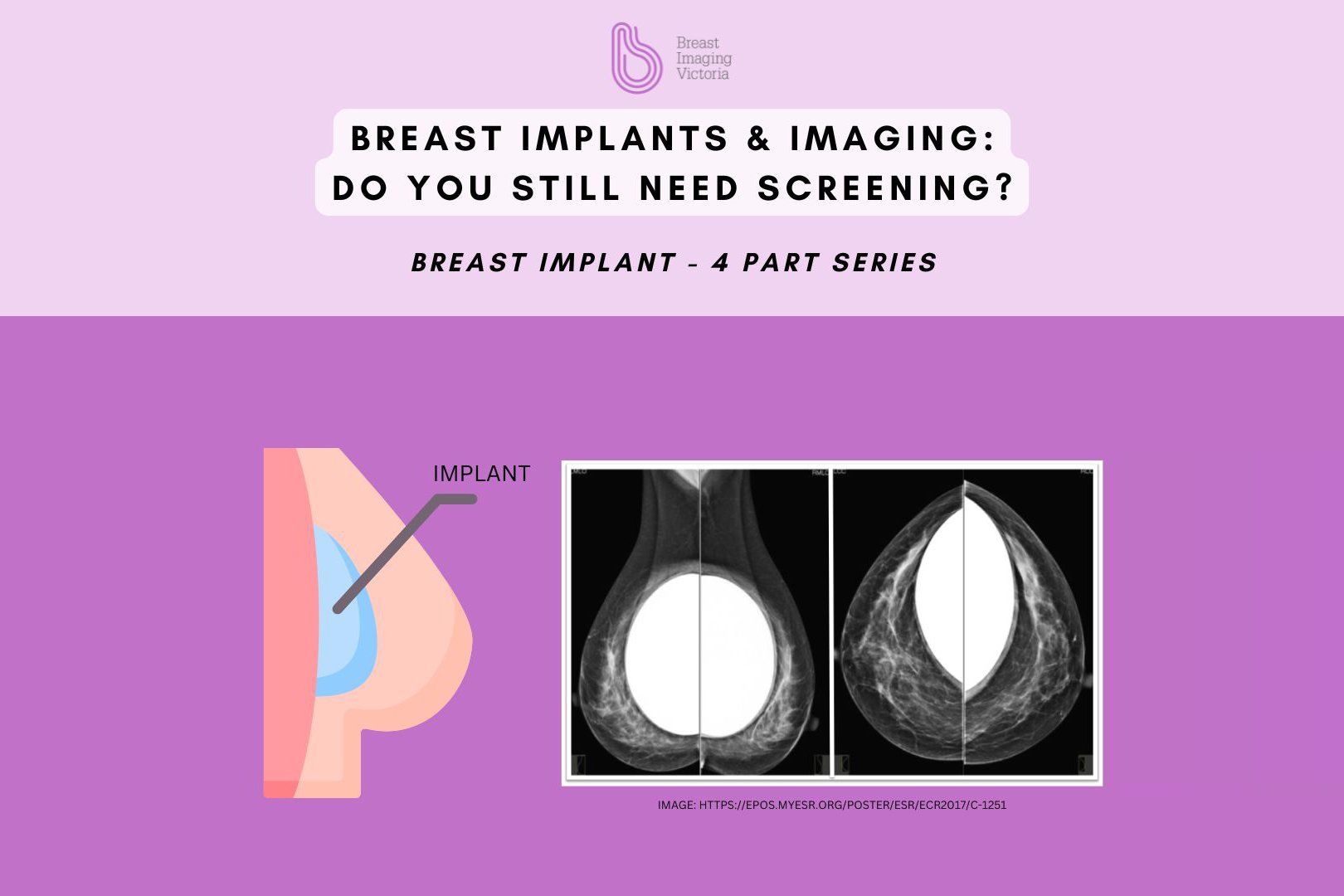
If you have breast implants, do you still need routine breast imaging? The answer is YES! - Breast implants don’t change your risk of breast cancer, you still have natural breast tissue that needs to be screened. - Mammograms + Ultrasound are typically done together at Breast Imaging Victoria to ensure a full assessment. - Mammograms require soft compression to keep the implant and breast tissue in place for clear images. Special techniques like implant displacement views help us capture as much breast tissue as possible. - Ultrasound is used alongside mammograms to check both breast tissue and implant integrity, as it provides a clearer look at any possible implant issues. MRI may be recommended for further evaluation if there are concerns about silent ruptures or hard-to-detect abnormalities. Why It Matters: Regular breast screening is just as important for women with implants. Cancer can develop in the breast tissue surrounding the implant, and early detection remains key. Got breast implants and unsure about screening? Our team is here to guide you through the process.
When it comes to breast biopsies, understanding the options can make the process less daunting. At Breast Imaging Victoria, we offer tailored biopsy techniques to ensure the most accurate results and best care: 🔍 Fine Needle Aspiration (FNA): - A quick, minimally invasive procedure under ultrasound, using a very thin needle to collect cells or fluid. - Commonly used for areas with fluid components, such as cysts or abscesses. - Provides fast results, making it ideal for straightforward fluid-related concerns. 🔍 Core Biopsy: - Uses a slightly larger needle to take a small piece of tissue from a solid lump for more detailed testing. - Done under ultrasound guidance for accuracy. - Provides key information to guide the next steps. 🔍 Stereotactic (Mammogram-Guided) Biopsy: - Performed for changes seen only on mammograms, like tiny calcium deposits (calcifications). - Uses mammography to pinpoint the area precisely. - Essential for investigating hard-to-see abnormalities. - The patient may be sitting or lying down depending on the location of the area. Every biopsy is chosen based on the unique findings from your imaging and your doctor’s recommendation. At Breast Imaging Victoria, we’re here to guide you through the process with care and expertise. If you have questions, don’t hesitate to reach out. We’re committed to helping you every step of the way.
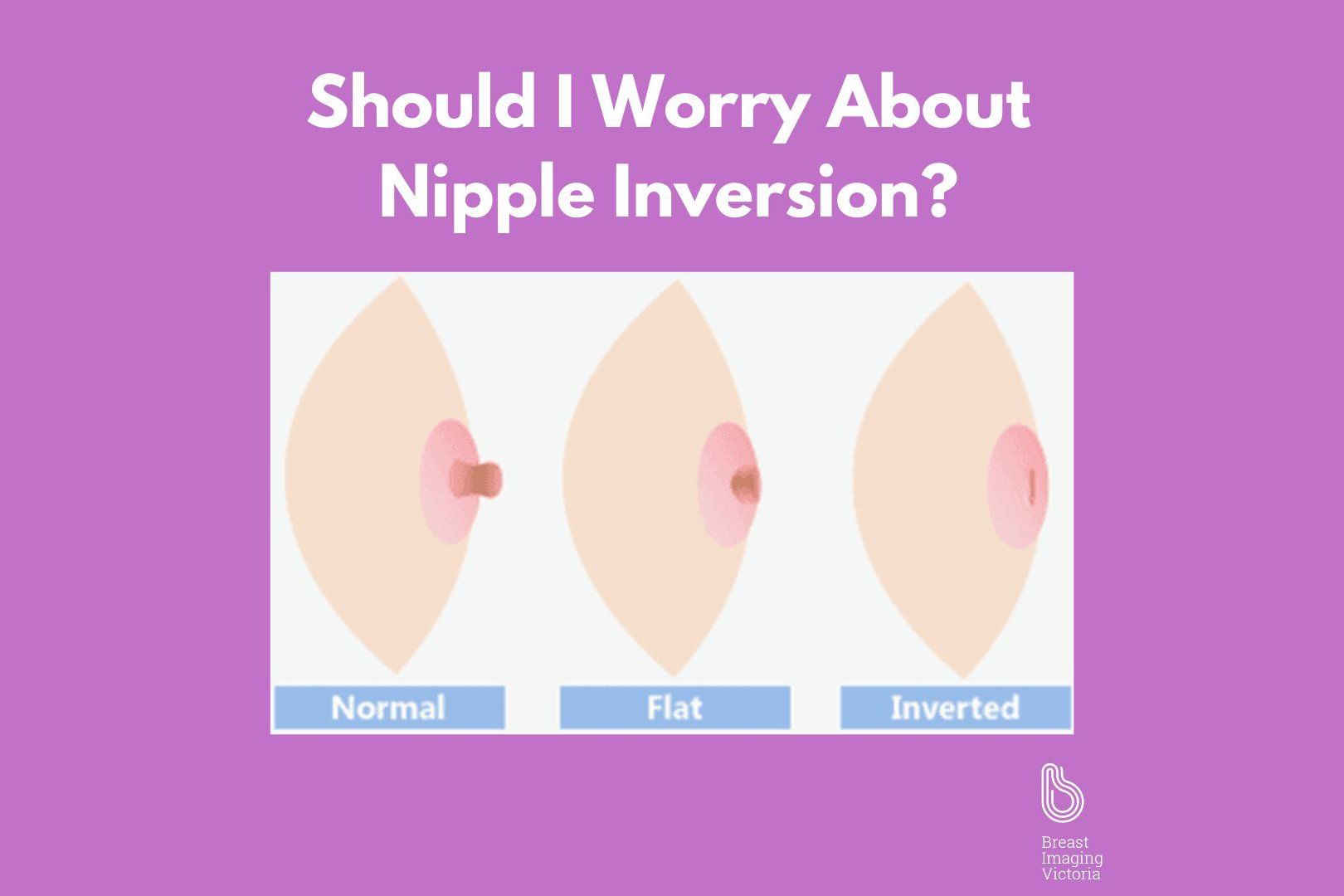
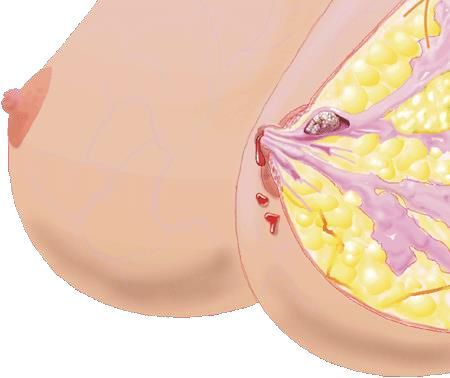
Nipple inversion, or retracted nipples, can be a natural anatomical variant or a concerning sign, depending on its onset and associated symptoms. At Breast Imaging Victoria, we are dedicated to educating our community about breast health and the significance of changes such as nipple inversion. What is Nipple Inversion? Nipple inversion refers to nipples that are turned inward rather than pointing outward. While some individuals may have congenitally inverted nipples, which are benign and present from birth, acquired nipple inversion, developing later in life, can sometimes signal underlying breast health issues. Potential Causes and Concerns : - Benign conditions: Infections or inflammations can alter breast tissue and lead to inversion. -Fibrocystic changes: These can cause non-cancerous lumps or thickened areas in the breast, pulling the nipple inward. - Breast cancer: Particularly concerning if the inversion is new, unilateral, and accompanied by other symptoms such as nipple discharge, breast lumps, or skin changes. Diagnostic Imaging and Evaluation: - Ultrasound and Mammography: Essential for assessing the underlying cause of nipple inversion, these imaging techniques help determine whether changes are benign or malignant. - MRI: Provides a more detailed view, recommended if there are additional risk factors or ambiguous findings from other imaging. When to Seek Medical Advice: If you notice new nipple inversion, especially if it's on one side only and accompanied by other symptoms like discharge or a lump, it's crucial to consult your doctor promptly. These signs can be indicators of serious conditions and should be evaluated as soon as possible. Our Commitment: At Breast Imaging Victoria, we’re committed to providing comprehensive breast care and ensuring our community is informed about potential breast health issues. Our team of specialists is here to support you in understanding and managing any breast changes.